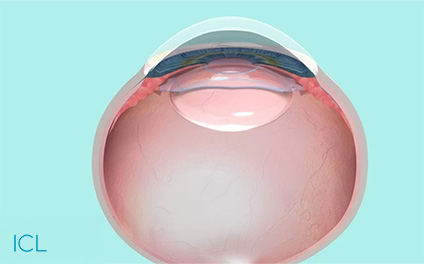
For those who would want something better than normal glasses or laser eye surgery, Implantable Contact Lenses (ICL) …
Dr. Natasha Lim Eye Centre – Laser Cataract & LASIK Surgery Singapore
Book an Appointment
It just takes a few minutes to book an appointment and we will get back to you with more details shortly.
Address:
#19-01/02/03/07/11
Royal Square Medical Centre
Royal Square @ Novena
101 Irrawaddy Road
Singapore 329565
-
#19-01/02/03/07/11 Royal Square Medical Suites
Royal Square @ Novena 101 Irrawaddy Road Singapore 329565.